Obesity Week 2013 Delayed or denied patients have higher mortality rate
Obesity Week 2013
Patients who were denied or delayed insurance approval for bariatric surgery, despite being cleared by their medical team, had a mortality rate three times higher than patients who received insurance approval without delay, researchers from University of North Carolina (UNC) have reported.
The research was presented at the 30th Annual Meeting for the American Society for Metabolic and Bariatric Surgery (ASMBS) during ObesityWeek 2013, the largest international event focused on the basic science, clinical application and prevention and treatment of obesity. The event was hosted by the ASMBS and The Obesity Society (TOS).
“For people with morbid obesity, bariatric surgery provides a significant survival benefit,” said study co-author Dr D Wayne Overby, a bariatric surgeon and Assistant Professor of Surgery at UNC Department of Surgery. “In this light, there seems to be no justification for employers, insurers or government payers to deny patients who meet evidence-based medical criteria from having access to it.”
According to the study, about one-in-five (22%) surgically eligible patients were initially denied by their insurance provider, and within a five-year period 6 percent of them died, compared to less than 2 percent of those who received insurance approval. The study followed 463 patients who were cleared for surgery by a multidisciplinary medical team (surgery, psychology and nutrition providers) from the UNC bariatric surgery program between 2003 and 2008.
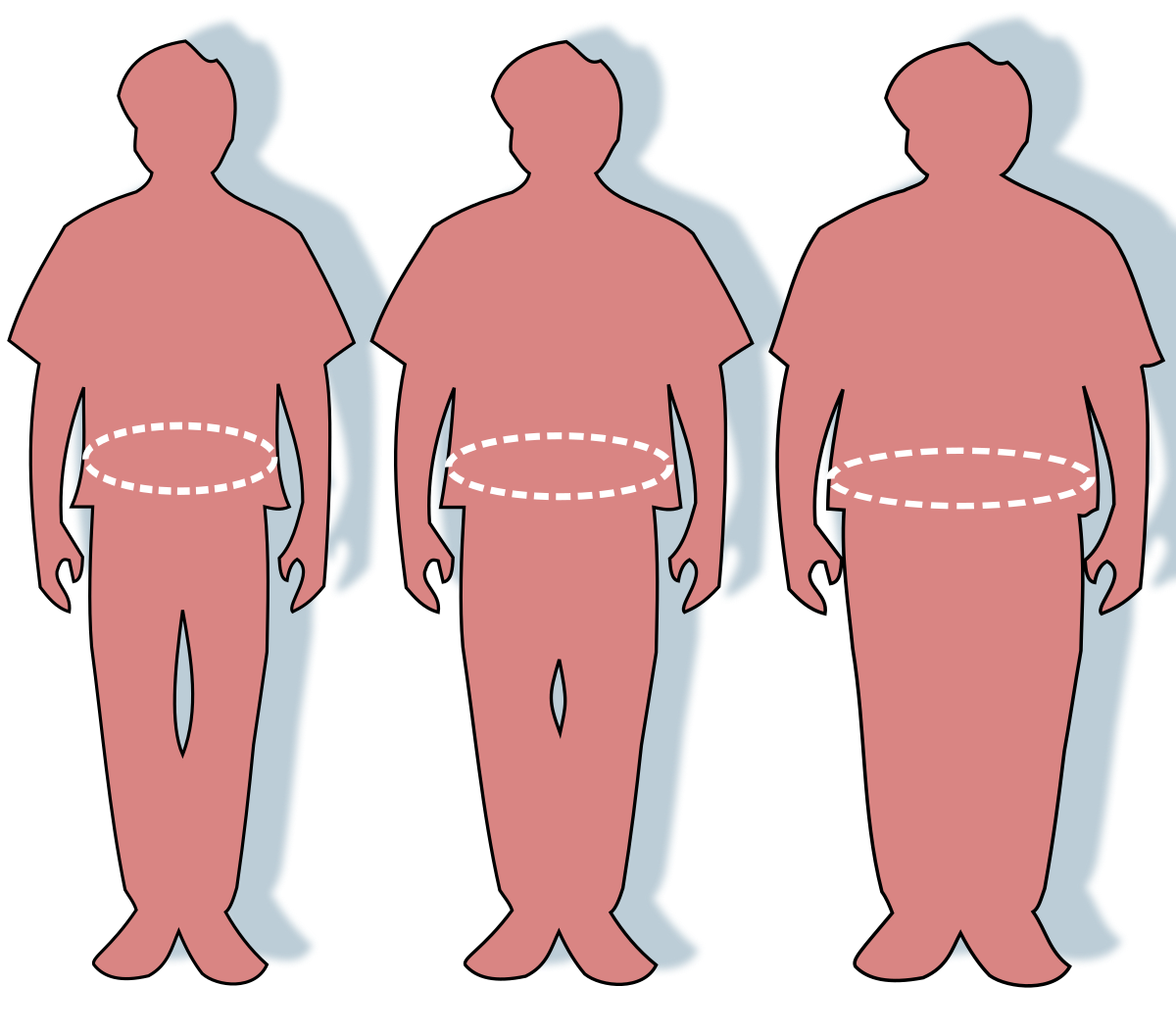
The study included 391 females and 72 males, whose average age was 45 and whose average BMI was 52.5. Nine of the 100 patients who were initially denied surgery were eventually able to overturn their denial and have surgery. UNC researchers measured patient mortality using the Social Security Death Index.
“Whether from uncontrolled obesity-related co-morbidities or from downstream treatment complications, reduced survival associated with denial or delay in bariatric coverage must be considered when implementing national and state policies around bariatric surgery,” said Dr Eleisha Flanagan, lead study author and Fellow in Minimally Invasive Surgery at UNC Hospitals.
Patients who lost more than 100lbs and those who lost weight through bariatric surgery had the highest risk of complications from later surgical procedures to reshape their bodies, a study from UT Southwestern Medical Center has reported.
“This is one of the first large-scale studies comparing outcomes in patients losing significant amounts of weight via surgical and nonsurgical means,” said Dr Jeffrey Kenkel, Professor and Acting Chairman of Plastic Surgery at UT Southwestern, and senior author of the study. “Major weight loss was a significant risk factor for wound complications in body contouring surgery.”

Dr Jeffrey Kenkel
The study, published in the Aesthetic Surgery Journal, compared surgical complication outcomes for 450 patients who underwent body contouring to remove excess sagging fat and skin to improve body shape.
Of the 450 study participants, 124 lost 50lbs or more before their surgery. Patients included men and women in all age groups who completed body contouring procedures including body lifts, tummy tucks, thighplasty, arm lifts, breast lifts, breast reduction, and liposuction.
The researchers conducted statistical analyses to identify risk factors and to determine the probability of patients experiencing healing issues or complications after their surgery.
Patients with weight loss of more than 100lbs were found to be at higher risk for complications, regardless of weight loss method. Furthermore, post-bariatric patients had the highest rate of complications; gastric bypass patients were at greater risk than patients who lost weight through diet and exercise, whereas patients who underwent gastric sleeve or the Lap-Band procedures had the lowest risk of complications among surgical weightloss patients.
“In addition to identifying massive weight loss patients as a vulnerable population, these types of studies are important to help surgeons improve patient care. The data that we have collected is valuable in managing known risks and designing pre- and post-surgical treatment,” said Kenkel.
With these considerations in mind, the researchers then investigated the physiological factors that make massive weight loss patients susceptible to complications, such as infection, delayed healing, ruptures, and reddening of the skin.
“It is imperative that patients account for their dietary deficiencies and prepare their bodies for surgery,” said Kenkel. “Nutrition plays an important role in skin healing, collagen production, and the generation of new blood vessels, all of which are important during recovery. Surgeons should monitor these patients carefully and make sure their vitamin and protein supplements are complete. Daily protein supplements are vital for achieving complication rates that are in line with non-bariatric candidates. We can also enhance recovery by tailoring pre-operative care to the patient’s weight loss amount and method. As our understanding of these risks advances, we are able to provide the growing number of body contouring patients the best possible circumstances for a safe recovery.”